The RESCUEicp Study
What's it about?
What did they do?
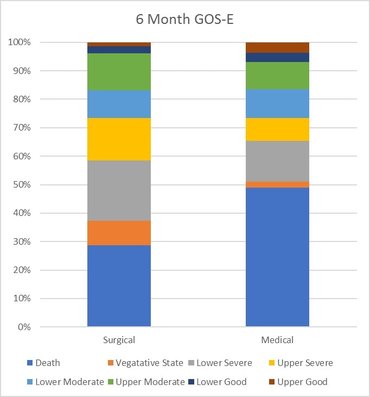
What did they find?
Is it any good?
Final THoughts
BW
Tom Heaton
Links & References
- Hutchinson P et al. Trial of decompressive craniectomy for traumatic intracranial hypertension (RESCUEicp Trial). 2016. NEJM. 375: 1119-1130. Avaialble at: http://www.nejm.org/doi/full/10.1056/NEJMoa1605215#t=article
- TheBottomLine. RESCUEicp. 2016. A great appraisal of the key points of the paper. Available at: http://www.thebottomline.org.uk/summaries/icm/rescue-icp/
- Cooper D et al. Decompressive craniectomy in diffuse traumatic brain injury (DECRA Trial). NEJM. 2011. 364: 1493-1502. Available at: http://www.nejm.org/doi/full/10.1056/NEJMoa1102077#t=article
 RSS Feed
RSS Feed
