
GAT ASM Homepage
Feedback
iWantGreatCare
Fantastic talk from Neil Bacon on iWantGreatCare. Convinced me about the benefits of transparent feedback #GATASM15
— Thomas Heaton (@tomheaton88) June 17, 2015
Excellence
Changing incident reporting to excellence reporting. 'Root cause of awesomeness' #GATASM15
— Thomas Heaton (@tomheaton88) June 17, 2015
If Disney Ran Your Hospital – Fred Lee
Wilful Blindness – Margaret Heffernan
Metacognition
Thinking Fast & Slow: Daniel Kahneman
The Chimp Paradox: Steve Peters
Results = Knowledge x Skills x performance
The idea behind this is that performance is everything. Elite athletes get one shot at this medal every 4 years. They will have spent hours each day developing the knowledge and skills to the maximum, but unless they perform on the day they will lose. I think the analogy is perfect for highly demanding clinical specialities such as anaesthesia and critical care, the main difference being that we have no idea when we need to perform. I might need to perform an emergency surgical airway tomorrow, or never do one in my whole career, but I still need to perform pretty well to avoid disaster. I have put together the knowledge and skills for such an event (I’ll opt for scalpel rather than needle - NAP 4) but have I really optimised my performance for what is almost certainly going to be a horrendous situation? Will I act quickly, calmly and decisively when this can’t intubate, can’t oxygenate scenario presents itself? I am a big fan of simulation for this reason and really wished we had more chance to do this on a regular basis (weekly?) but Tom described how the world’s top, highest fidelity simulator remains the human mind. Top athletes visualise crossing that line in first place as a core part of their training. I think I will be spending a bit more time thinking about all the most horrific things that can go wrong, and how they shall be resolved in a calm and decisive manner. I don’t really want the real time to be the first time.
Clinical
And Finally...
Major haemorrhage more common than CICO scenario but not as much focus on it in our training #GATASM15
— Thomas Heaton (@tomheaton88) June 17, 2015
Tom Heaton
Links
iWantGreatCare
If Disney Ran Your Hospital – Fred Lee
Wilful Blindness – Margaret Heffernan
Safety I & Safety II - Erik Hollnagel
Metacognition
Thinking Fast & Slow: Daniel Kahneman
The Chimp Paradox: Steve Peters
From Mindless to Mindful Practice
Clinical Cognition & Diagnostic Error
Clinical
Prevention of atelectasis
The PROPPR Trial
Skeletal Muscle Mitochondria Paper
CESAR Trial
Diastolic Dysfunction
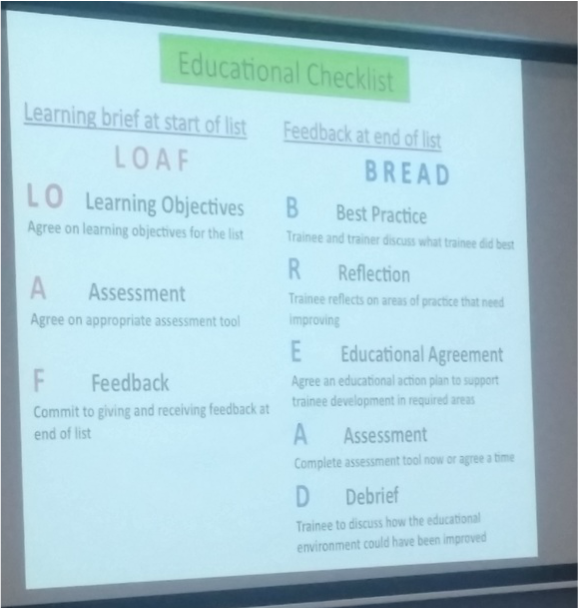
Education
Adult Learning Theories
 RSS Feed
RSS Feed
